Farming For Life
Farming for life: impact of medical prescriptions for fresh vegetables on cardiometabolic health for adults with or at risk of type 2 diabetes in a predominantly Mexican-American population
The Problem:
Poor diet is the leading cause of poor health in USA, with fresh vegetable consumption below recommended levels. We aimed to assess the impact of medical prescriptions for fresh (defined as picked within 72 hours) vegetables, at no cost to participants on cardiometabolic outcomes among adults (predominantly Mexican-American women) with or at risk of type 2 diabetes (T2D).
Our Solution:
Between February 2019 and March 2020, 159 participants (122 female, 75% of Mexican heritage, 31% with non-insulin treated T2D, age 52.5 (13.2) years) were recruited using community outreach materials in English and Spanish, and received prescriptions for 21 servings/week of fresh vegetable for 10 weeks. Pre-post comparisons were made of weight; waist circumference; blood pressure; Hemoglobin A1c (HbA1c, a measure of long-term blood glucose control); self-reported sleep, mood and pain; vegetable, tortilla and soda consumption. After obtaining devices for this study, 66 of 72 participants asked, agreed to wear blinded continuous glucose monitors (CGM).
Figure 1. Participation flow between February 2019 and March 2020. Note: Recruitment and follow-up visits were cancelled after March 2020 due to the COVID-19 pandemic. CGM, continuous glucose monitors.
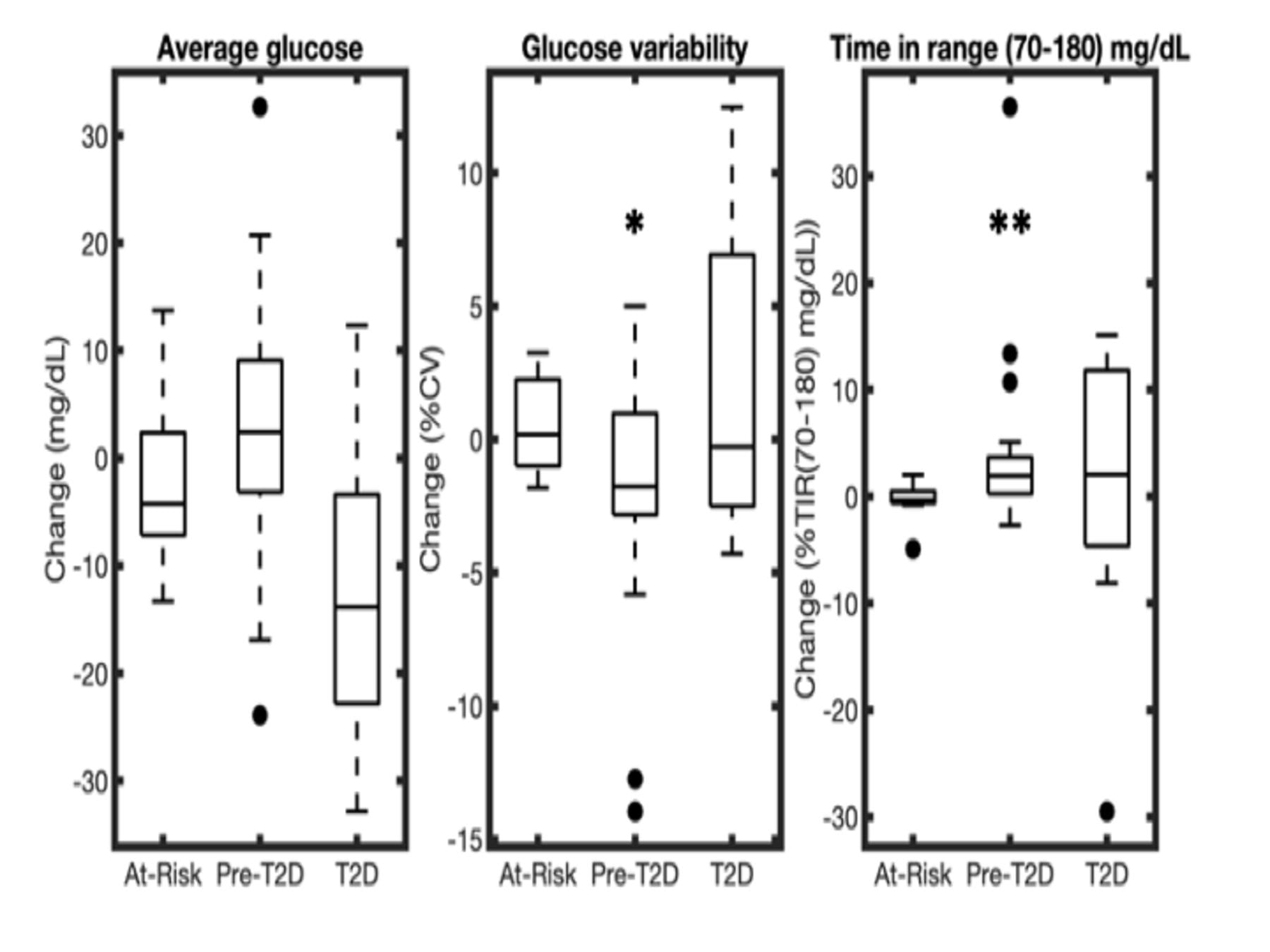
Figure 2. Change in average glucose, glucose variability measured as the percentage coefficient of variation (%CV) and time in range (TIR) (70–180 mg/dL) for n=40 participants wearing CGM at baseline and at 3 months. Participants are stratified by baseline HbA1c at baseline into at-risk (HbA1c < 5.7%), pre-T2D (HbA1c 5.7%–6.4%), and T2D (HbA1c > 6.4%). A positive value represents an increase of the CGM variable from baseline to 3 months, while a negative value represents a corresponding decrease. Results are shown as box plots (*p<0.05, **p<0.01). CGM, continuous glucose monitor; T2D, type 2 diabetes.
Results:
Paired data were available for 131 participants. Over 3 months, waist circumference fell (−0.77 (95% CI −1.42 to 0.12) cm, p=0.022), as did systolic blood pressure (SBP) (−2.42 (95% CI −4.56 to 0.28) mm Hg, p=0.037), which was greater among individuals with baseline SBP >130 mm Hg (−7.5 (95% CI −12.4 to 2.6) mm Hg, p=0.005). Weight reduced by −0.4 (−0.7 to –0.04) kg, p=0.029 among women. For participants with baseline HbA1c >7.0%, HbA1c fell by −0.35 (-0.8 to –0.1), p=0.009. For participants with paired CGM data (n=40), time in range 70–180 mg/dL improved (from 97.4% to 98.9%, p<0.01). Food insecurity (p<0.001), tortilla (p<0.0001) and soda (p=0.013) consumption significantly decreased. Self-reported sleep, mood and pain level scores also improved (all p<0.01).
Conclusions:
Medical prescriptions for fresh vegetables were associated with clinically relevant improvements in cardiovascular risk factors and quality of life variables (sleep, mood and pain level) in adults (predominantly Mexican-American and female) with or at risk of T2D.
Team

David Kerr
Director of Research and Innovation
Sansum Diabetes Research Institute

SOUPTIK BARUA
Postdoctoral Fellow, ECE
Rice University

Namino Glantz
Associate Director, Mil Familias Programs
Sansum Diabetes Research Institute

Casey Conneely
Research Assistant
Sansum Diabetes Research Institute
Mary Kujan
Sansum Diabetes Research Institute

Wendy Bevier
Research Associate
Sansum Diabetes Research Institute

Arianna Larez
Logistics Lead
Sansum Diabetes Research Institute

Dr. Ashutosh Sabharwal
Professor
ECE, Rice University
