Novel signatures for Type-2 diabetes progression using continuous glucose monitoring
Daytime glucose signatures for early prediction of type 2 diabetes onset and progression in adults with or at risk of type 2 diabetes in a predominantly Mexican-American population
The Problem:
Continuous glucose monitoring (CGM) has been shown to be beneficial for people living with diabetes, but the supporting evidence is almost exclusively from White individuals with type 1 diabetes. In this project, we are quantifying CGM profiles and assessing the applicability/benefits of CGM in Hispanic/Latino adults with or at-risk of non-insulin treated type 2 diabetes (T2D).
Our Solution:
We conducted a study in 100 participants (79 female, 86% Hispanic/Latino [predominantly Mexican], age 54·6 [±12·0] years). The study participants wore blinded CGMs for 2 weeks. The participants were stratified into (i) at risk of T2D, (ii) with pre-diabetes (pre-T2D), and (iii) with non-insulin treated T2D. Beyond standardized CGM measures (average glucose, glucose variability, time in 70–140 mg/dL and 70–180 mg/dL ranges), we also examined additional CGM measures based on the time of day.

Time in 140 to 180 mg/dL range stratified by group and time (overnight versus rest of day). At-risk participants denoted using blue dots, pre-T2D participants using green dots, and T2D participants using red dots. The 45∘dotted line indicates equal values for overnight and rest of day time in 140 to 180 mg/dL range.
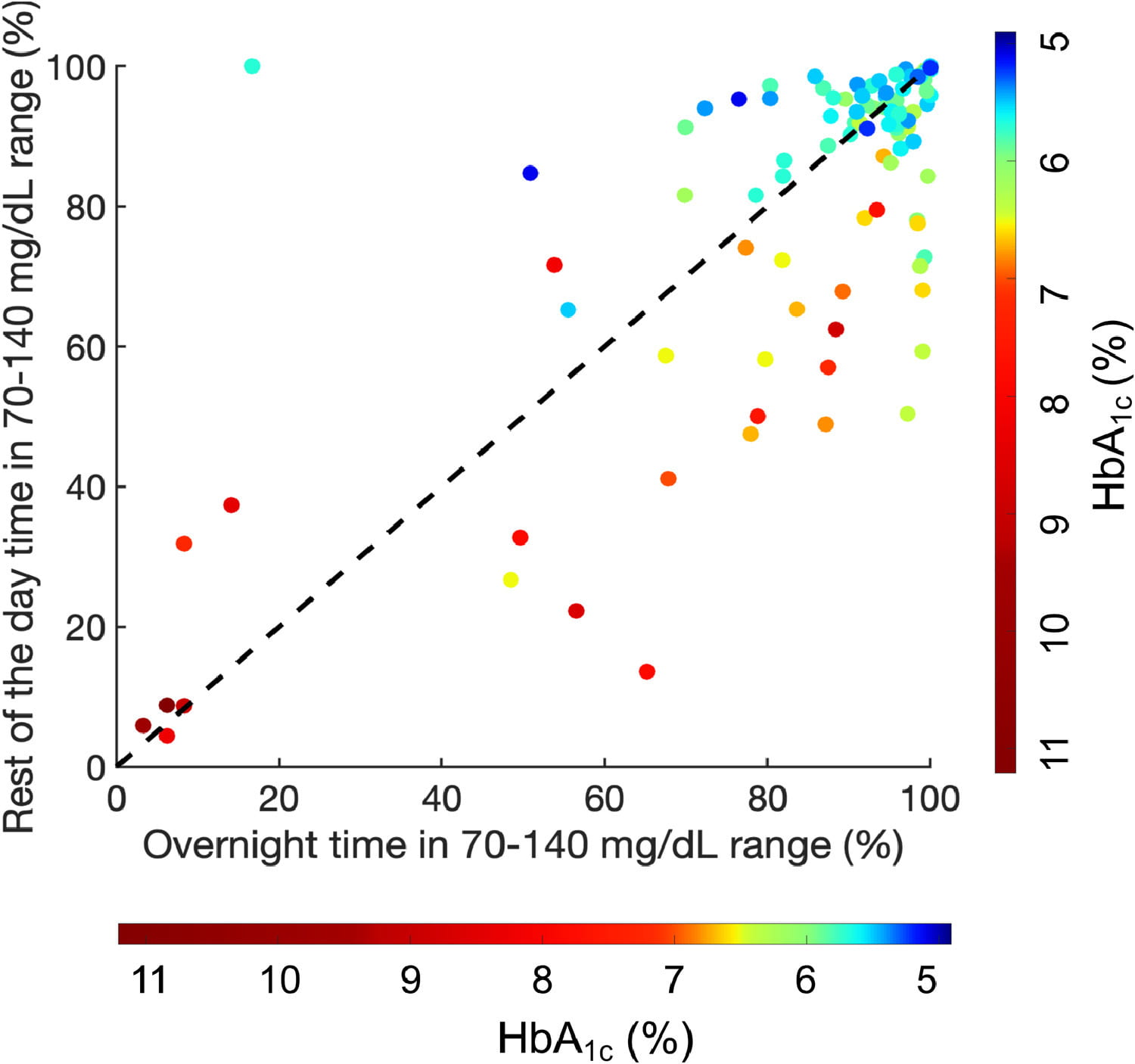
Relationship between overnight and rest of the day time in 70–140 mg/dL range with HbA1cfor all participants. Color bar representing HbA1cvalues varies from 5.0%(dark blue) to 11.0% (dark red). The 45∘dotted line indicates equal values for overnight and rest of day time in 70–140 mg/dL range.
Results:
Standardized CGM measures were significantly different for participants with T2D compared to at-risk and pre-T2D participants (p<0·0001). In addition, pre-T2D participants spent more time between 140 and 180 mg/dL during the day than at-risk participants (p<0·01). T2D participants spent more time between 140 and 180 mg/dL both during the day and overnight compared to at-risk and pre-T2D participants (both p<0·0001). Time in 70–140 mg/dL range during the day was significantly correlated with HbA1c (r=-0·72, p<0·0001), after adjusting for age, sex, BMI, and waist circumference (p<0·0001).
Conclusions:
Standardized CGM measures show a progression of dysglycemia from at-risk of T2D, to pre-T2D, and to T2D. Stratifying CGM readings by time of day and the range 140–180 mg/dL provides additional metrics to differentiate between the groups.
Team

SOUPTIK BARUA
Postdoctoral Fellow, ECE
Rice University

Dr. Ashutosh Sabharwal
Professor
ECE, Rice University

Namino Glantz
Associate Director, Mil Familias Programs
Sansum Diabetes Research Institute

Casey Conneely
Research Assistant
Sansum Diabetes Research Institute

Wendy Bevier
Research Associate
Sansum Diabetes Research Institute

Arianna Larez
Logistics Lead
Sansum Diabetes Research Institute

David Kerr
Director of Research and Innovation
Sansum Diabetes Research Institute
